
Despite this improvement in survival, it is clear that autologous stem cell transplant (auto- SCT) is not curative in the majority of patients. Although this has been proven in only one randomized trial, the results of several phase II studies provide a substantial body of evidence favoring the use of high-dose therapy (recently reviewed by Fassas and Tricot). Newly diagnosed multiple myeloma patients treated with high-dose chemotherapy and stem cell transplantation have a superior outcome in terms of eventfree and overall survival, compared with conventional chemotherapy recipients. Until the efficacy and safety of this procedure is fully established, it should be limited to high-risk patients.

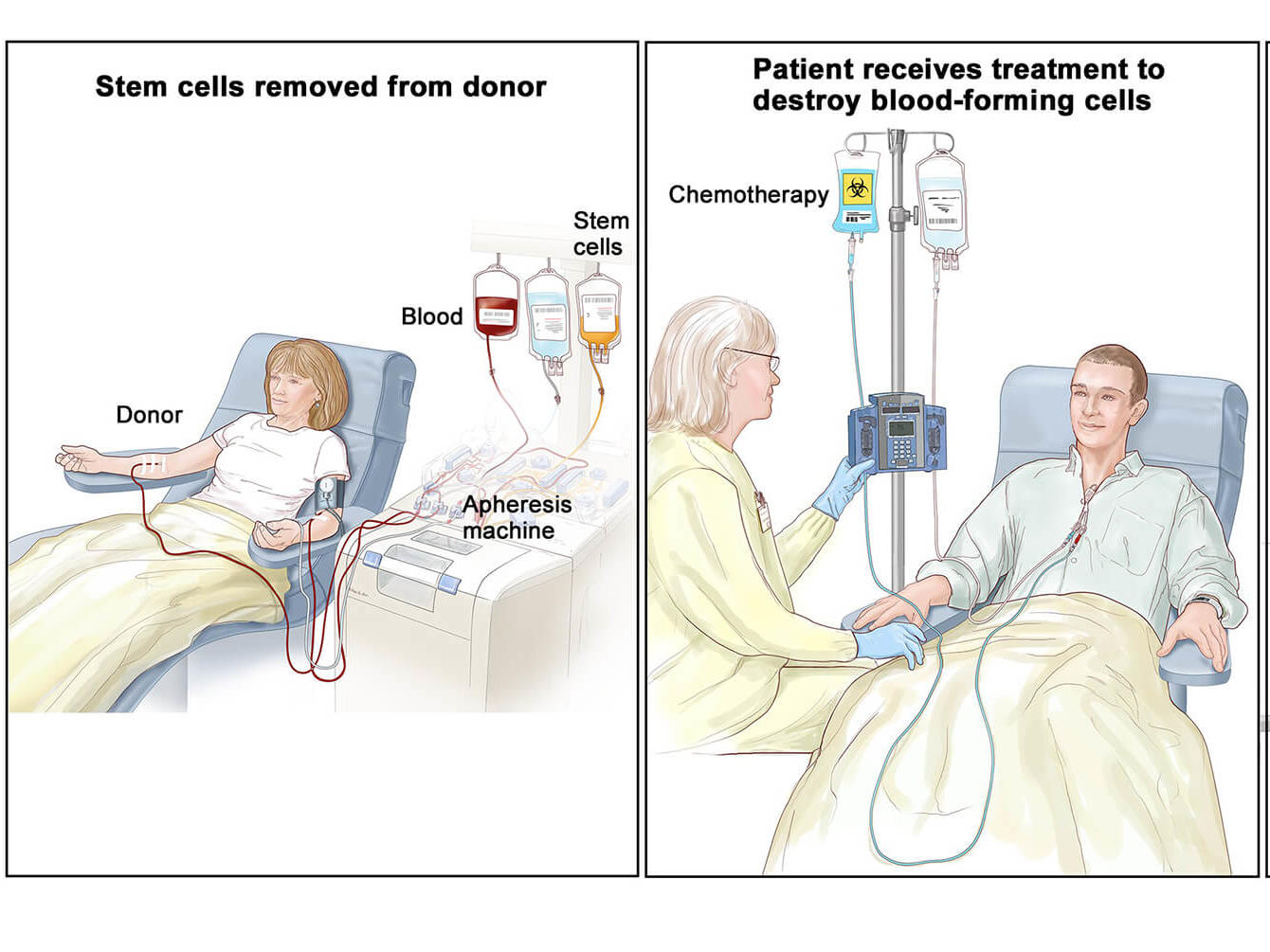
High-risk patients (defined by chromosomal abnormalities usually involving chromosomes 11 and 13 and high beta-2-microglobulin levels) whose median survival after tandem transplant is less than 2 years should be offered novel therapeutic interventions such as tandem "auto/allo" transplants. Good-risk patients (defined by normal cytogenetics and low beta-2-microglobulin levels), especially those who achieve a complete or near-complete response after the first transplant, appear to benefit the most from a second cycle. A central issue of tandem transplants, whether they involve autologous or allogeneic transplants, revolves around defining the subsets of patients who will benefit from the procedure. The recent reports of tandem autologous transplant for maximum cytoreduction followed by nonmyeloablative allogeneic transplant for eradication of minimal residual disease appears promising and deserve further investigation. An additional high-dose chemotherapy course (with tandem transplants) appears to improve progressionfree survival, although the effect is not discernible until 3 to 5 years posttransplant. Despite these results, autologous transplantation has not changed the ultimately fatal outcome of the disease, as there is no substantial evidence of "cure" in most published studies. In newly diagnosed patients, complete remission rates of 25% to 50% can be achieved, with median disease-free and overall survivals exceeding 3 and 5 years, respectively. Until theefficacy and safety of this procedure is fully established, it should belimited to high-risk patients.ĪBSTRACT: The use of high-dose chemotherapy and autologous stem cell support in the past decade has changed the outlook for patients with multiple myeloma. High-risk patients (defined bychromosomal abnormalities usually involving chromosomes 11 and 13and high beta-2–microglobulin levels) whose median survival aftertandem transplant is less than 2 years should be offered novel therapeuticinterventions such as tandem “auto/allo” transplants. Good-risk patients (defined by normal cytogeneticsand low beta-2–microglobulin levels), especially those who achievea complete or near-complete response after the first transplant, appearto benefit the most from a second cycle. A central issue of tandemtransplants, whether they involve autologous or allogeneic transplants,revolves around defining the subsets of patients who will benefitfrom the procedure.
:max_bytes(150000):strip_icc()/GettyImages-1092323846-a4a95e9263c84165b7d76b8bd5def4cc.jpg)
The recent reports of tandem autologous transplant formaximum cytoreduction followed by nonmyeloablative allogeneictransplant for eradication of minimal residual disease appears promisingand deserve further investigation. An additional high-dose chemotherapycourse (with tandem transplants) appears to improve progressionfreesurvival, although the effect is not discernible until 3 to 5 yearsposttransplant. Despite theseresults, autologous transplantation has not changed the ultimatelyfatal outcome of the disease, as there is no substantial evidence of“cure” in most published studies. In newly diagnosed patients, complete remissionrates of 25% to 50% can be achieved, with median disease-free andoverall survivals exceeding 3 and 5 years, respectively.
The use of high-dose chemotherapy and autologous stem cellsupport in the past decade has changed the outlook for patients withmultiple myeloma.


 0 kommentar(er)
0 kommentar(er)
